Surgery for Pilonidal Cyst
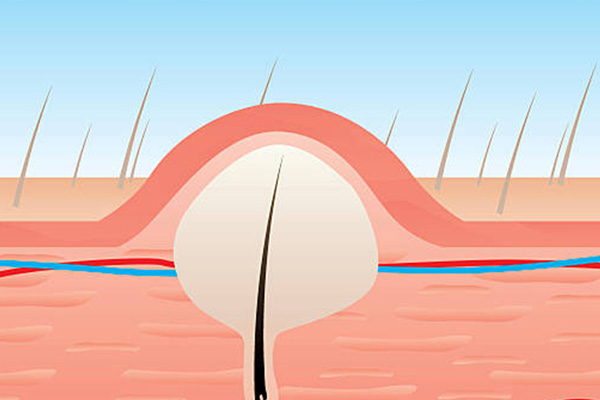
A pilonidal cyst is a pocket filled with fluid that also contains body hairs found at the natal cleft just right below the coccyx. It could either be symptomatic presenting with pain due to infection or an inflammation or asymptomatic. It most commonly occurs in men of the Caucasian race.