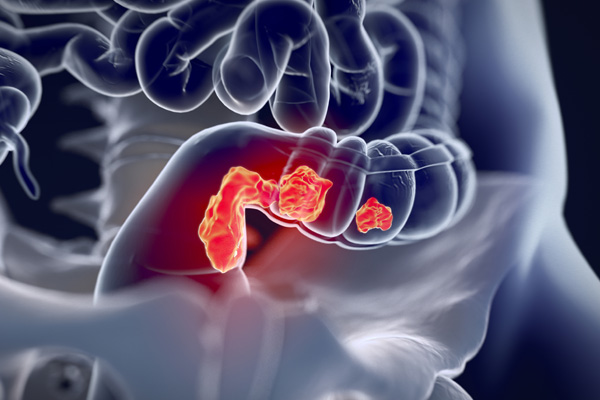
What is Rectal Cancer?
Rectal cancer is the cancer of the rectum, which is the lowermost part of the digestive system. Rectal cancer is often referred in combination with the colon as colorectal cancer.
According to the Centers for Disease Control and Prevention (CDC), colorectal cancer is the second leading cause of cancer deaths in the United States. It is estimated that 1 in 20 (5%) persons will develop colorectal cancer during their lifetime in the US.