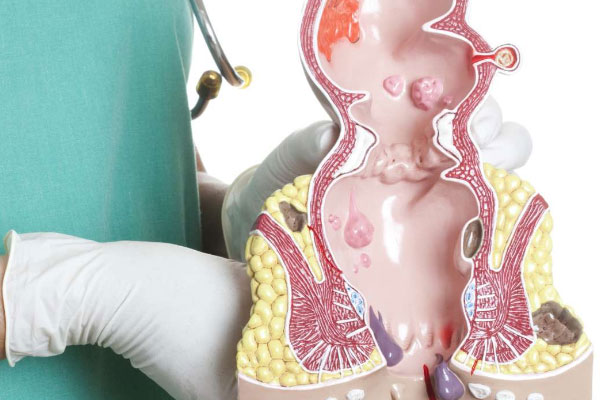
Hemorrhoidectomy
Hemorrhoids are a collection of blood in the venous system (engorged veins) that occurs in the anal region either internally or externally.Hemorrhoidectomy is normally reserved for the failed outpatient treatment but factors such as the patient’s preference, the extent of the clinical signs and symptoms and the anatomy of the hemorrhoid are also considered when considering surgery.